Making A Difference And Loving What You Do- Bree Johnson
In this episode, we have Bree Johnson. She's a third generation EMT. That means her mom, her dad, her cousin, and uncle have all been in fire and EMS, which is pretty impressive. Bree did not want to be an EMT when she's younger, but somehow, she was convinced. And that seems to be her calling. Bree is also working as a flight dispatcher and an ER tech. And if that wasn't enough, she's going to school to be a respiratory therapist. Let's dive down into the episode and listen to how Bree juggles all this stuff going on in her life. Plus has an amazing outlook on how to handle her mental health.
In this episode, we have Bree Johnson. She's a third generation EMT. That means her mom, her dad, her cousin, and uncle have all been in fire and EMS, which is pretty impressive. Bree did not want to be an EMT when she's younger, but somehow, she was convinced. And that seems to be her calling. Bree is also working as a flight dispatcher and an ER tech. And if that wasn't enough, she's going to school to be a respiratory therapist. Let's dive down into the episode and listen to how Bree juggles all this stuff going on in her life. Plus has an amazing outlook on how to handle her mental health.
In this episode, we can learn:
👉 What it's like to be with a family of first responders;
👉 How to balance work, school, and personal life;
👉 How to build confidence in you and your patient while taking care of them;
👉 Mental health care is a must;
👉 First responders have limitations too;
👉 How to distinguish okay and not okay scenes in our job;
As a First Responder, you are critical in keeping our communities safe. However, the stress and trauma of the job can take a toll on your mental health and family life.
If you're interested in personal coaching, contact Jerry Lund at 435-476-6382. Let's work together to get you where you want to be to ensure a happy and healthy career.
Podcast Website www.enduringthebadgepodcast.com/
Podcast Instagram www.instagram.com/enduringthebadgepodcast/
Podcast Facebook www.facebook.com/EnduringTheBadgePodcast/
Podcast Calendar https://calendly.com/enduringthebadge/enduring-the-badge-podcast
Personal Coaching https://calendly.com/enduringthebadge/15min
Host Instagram www.instagram.com/jerryfireandfuel/
Host Facebook www.facebook.com/jerrydeanlund
Hi, everyone, and welcome to this week's episode of Enduring the Badge Podcast. I'm your host Jerry Dean Lund and I don't want you to miss an upcoming episode, so please hit that subscribe button. And while your phones out, please do me a favor and give us a review on iTunes or Apple podcasts. It says, Hey, this podcast has a great message and we should send it out to more people. So please take that 30 seconds to a minute to do that review. And just maybe by doing that, it will push this up into someone's podcast feed that really needs this message.
My very special guest today is Bree Johnson. She's a third generation EMT. That means her mom, her dad, her cousin, and uncle have all been in fire and EMS, which is pretty impressive. Bree did not really want to be an EMT when she's younger, but somehow, she was convinced. And that seems to be her calling. Bree is also working as a flight dispatcher and an ER tech. And if that wasn't enough, she's going to school to be a respiratory therapist. Let's dive down into the episode and listen to how Bree juggles all this stuff going on in her life. Plus has an amazing outlook on how to handle her mental health. How're you doing Bree?
I'm doing well. How are you?
I'm doing great, too. And we were just chatting before we got started. Do you have some, his would be great in the video for sure if everyone watches this. Yes. And visitors in the background that wanting some attention?
Oh, yes, they are very much. They crave attention at all times. And we're not going to mine. Until tomorrow. My parents. Oh, no, sorry.
Yeah. So you have four dogs. That's a lot to handle.
Yes. Luckily, only two of them are mine. The other two are my parents. But when they're all together, they can get a little rowdy. And then they love to play.
So yeah, I would imagine.
Hopefully they behave right now.
I'm sure that'd be great. Bree, tell the audience a little bit about yourself.
Um, well, I don't even know where to start. Um, I guess a quick little rundown about me is I currently have a very unique dynamic going on with my life. Full time, I do aeromedical dispatching for Memorial Hermann life light. In Houston, Texas, which is honestly, a really great organization to work with. It was the first air medical company in the state of Texas hospital base. So they're actually just celebrating their 45th anniversary. So getting on with them was like a dream come true. I also worked part time as a advanced EMT on a 911 service. And I love that, too. It's two different sides of Emergency Medicine. Yeah. So it definitely gives a great overview of everything. And if that wasn't enough, I'm also in school full time for Respiratory Therapy./respiratory-therapist-526063_HL-7cd2f0630d764c7bbcb735c7840cd4aa.png)
Wow, how do you handle all three of those?
Very, very interestingly, I guess, to say I work at night. So I'm full time night shift. And I go to school during the day. So there's a lot of sleepless days that I know in the end will be worth it. And then it's kind of plugging in my EMS job when I can. Yeah, I'm not ready to give that up yet. I love being out on the streets.
Yeah, where is that out? In Texas they're out on the streets.
Um, so it's, I run in a little city called Highlands, Texas. It's just east of downtown Houston. Okay. I'm horrible with miles, but probably it's about 30 minutes outside of downtown Houston. So it's just like this little blink and you miss it city. But it's fun. There's definitely a lot of interesting calls. A lot of interesting people. I think if you talk to anyone on my department that say the same thing, very unique little city that you wouldn't think a lot of stuff happens, but a lot of stuff happens.
Yeah, yeah. As you blink by those cities, you just don't know. Right? Exactly. So do you do you actually use the your their medical service out there?
I do. Yeah. So that little area is controlled by all the same, like dispatch, and we actually have a really good relationship with they're called Econ EES. Harris County communications, I think. But yeah, overall, over on the east side of Houston. They actually work really, really, really well with Memorial Hermann lifeflight. So it's fun when I'm working on 911. And I get to call them and do a little tag team and I'm like, go
Yeah, that's very unique. It's to have that opportunity to do that. Yes. So how long have you been in EMS?
I've been an EMS now going on six years. July of this year, we'll make six years. So I've been a basic four, four of those. And then last year, actually, just a year ago, I finished up with my testing for advanced EMT. So
Awesome. Is that been that long? Yeah. Is that the highest level of certification out in your area?
No, paramedic is. But in Texas. And hopefully, I'm not getting this wrong. You have to go through advance in order to get to the paramedic, right. And at my school, it was like the last class where you could test out in advance before, like, having to go through paramedic. So I actually tested out nationally in advance, and decided that that's where I would stop for now. For now, as I go back,
yeah, yeah. I mean, you got some free time. Right? in between? Yeah. Two jobs in school. Yeah. All the time in the world.
Let's just throw another full time school in there.
Yeah, how long with your full time school? How long is that going to take before you graduate?
Um, so my program runs straight through semester wise. So I started in January of this year, and it'll run through the summer semester into fall, and I will be done in August of next year. So it's a year and a half or five semesters.
Wow. Yeah, that's a lot of learning and a lot of juggling those jobs while you're trying to learn.
It is it's yeah.
How do you handle? Yeah, I mean, just kind of throw out what your what does your day normally look like? Because if you're working and going to school, and like, are you sleeping and surviving and thriving in your own personal life?

Well, that's the fun thing is I don't really have much of a personal life right now, because I am so dedicated to working in school. But I think my schedule for my dispatching job, it's great. It can be hard sometimes. But it's great. We do a five on five off two on two on schedule. So I work five days in a row. I'm off for five days. I'm on for two days. And then I'm offered to say that right? five on five off to one two off. Yeah. So during those five days, it's a little bit difficult with school, because I'm going straight from school, or from work to school, sleeping for about two hours, and then getting up and getting ready to go back to work again. Wow. Yeah, but that's only three days a week that I have to do that. So it's not terrible when I work both five days. But it can be a little challenging.
Yeah. Sleep wise. Yeah, that I bet that that would be very, very difficult. Those those days. Do you ever get a chance to sleep in and make that sleep time up?
Um, so luckily, my classes there on Monday, Tuesdays and Thursdays so on Wednesdays, I get a full day of sleep. So I kind of just have to power through the Monday and Tuesday to get to Wednesday. And it's kind of like a little incentive to me that I guess. Yeah, go and sleep all day. But usually I don't get to like sleeping. Right. There's a lot of traffic in Houston's. So sleeping in really isn't an option. And I live about 30 minutes south of the Texas Medical Center where my dispatch centers located. So it's driving to there that it's always a fun drive with how much traffic there is.
Yeah, yeah. I think every city in America is exploding. I've I've been in Houston before too. Yeah. And the traffic and have family that lives in Houston. They always talk about Yeah, it's maybe just a few miles away, but it takes forever to get there.
Yes, it's like it. I think someone said it takes like two hours to get from one end to the other end of Houston. And that is so true. With just how much traffic There's downtown. I don't even go to downtown. That's not my part of town.
So, Bree, you have like a look what got you into EMS, you have a like some some people in your family that kind of looks like I might have inspired you to do that.
I do I I come from a family of first responders. My so currently my dad is a firefighter EMT. My uncle is also a firefighter EMT. They're both paramedics. So they've got the highest batch. My mom used to be a firefighter EMT. My grandpa used to be one. I've got a cousin who's a paramedic, so it kind of just all aligned one day and if you asked my family they would never have seen me in EMS. one bit. They kind of laughed at me when I told them that I wanted to switch career fields and join the EMS world.
Alright, well, I'm gonna have to ask, why would they say that?
Because I was never that. So if you sat me in my sister down, you know, probably seven, eight years ago, and you put a picture of, you know, a bloody car wreck, for instance, in front of us, I would be the one that would be cringing, and my sister would be all over it. And then all of a sudden, like, the roles reversed. And so now if you put like a bloody car wreck in front of us, like I'm like, oh, yeah, like, Let's go like, I'm so ready. And my sister's like, No, you guys have fun with that. And so she'll just listen to me and my dad talk about these things. And she's like, Yeah, she's going to school to be a radiology techs. So she's got to eventually see stuff like this. But she's like, I'll let you guys handle the outside of the hospital part. And I'll just take pictures.
Yeah, it'll probably be a little bit of a cleaner operation inside the radiology area a little bit. And that's, that's great thing about, you know, EMS is you. It's not meant for everybody, right? They're just a certain thrilling people that feel like they have a calling to do that.
And my I, honestly, I mean, if you would have asked me probably seven years ago, I would have been like, No, I have no interest. In doing EMS, I was actually actually went to school and have an associate's degree in baking and pastry arts. And that's what I was doing for probably about four or five years. And then it wasn't until actually my grandpa passed away. And we were on family vacation with my uncle, who's the paramedic, and we're sitting on the beach one day, and my uncle is like, why don't you go to school to be an EMT. And I was like, because I don't want to, I had no urge to. And then, six weeks after my grandpa passed away, my aunt actually died in a car accident, all from the same side of the family. And so I think, after that moment, I was like, You know what, I need to do something a little bit more with my life, other than bake bread and cupcakes and decorate cakes, and I put in an application for the EMT program. And initially, I was waitlisted into that class, or that round of classes. And then I got a call.
Hey, everyone, I want to thank my sponsor, Responder Wipes. They're the best econ wipes on the market far superior than any others out there. I love how thick and durable these wipes are. They're very safe, you can use them from head to toe and everywhere in between, the wipes are extra wet and leave you feeling fresh and clean. They also can be used as a cooling towel, almost incredibly hot days or after an incident that gets you overheated. Please check them out at responder wipes.com and follow them on Instagram, probably about
A month before school started so that they have a spot for me. So it was kind of just a sign that it was meant to be.
Yeah, yeah, that's that is quite a change. though. I'm sure people really love if you actually share some of those skills at work about baking bread and bringing in some cupcakes and stuff. I would really love it.
When they find out that I can bake. They are like alright, well, when are you going to bring in something? And I'm like, Well, I don't much like baking anymore. Because when you do it for so, so long. I don't know why I thought I could make a career out of that. At the time, I loved it. But now looking back, I'm like, I don't think I could have made a life with baking. Just has more power to the people who can because Right, right? I'm just not one of those people turns out, no, I just have this degree that sits on the shelf.
Someday, you just never know you might be able to use it for something that maybe interacts with EMS. Who knows?
It could I have made several cakes for are like staff meetings over at lifelight. So people have enjoyed it. But yeah, now I don't do that much anymore, especially with COVID. I mean, after COVID We stopped having in person meetings for a while. And so I kind of got off the hook from having to make cakes.
Right? So listening probably to all your family members discuss all these calls that they've gone on and probably you know, when you share calls like that they're not always the best calls that they're sharing. That didn't deter you away from this field.
No. I saw like yawns and it just sounded really funny. But no, I guess like I've seen my dad come home after some pretty hard calls. And I've had to find myself as like a high school or help my dad handle some of these rougher calls that he's come home from because you know, my brother was in the military. And so I remember one time my mom was out in San Diego when my brother was coming home from one of his deployment And I was home with my dad. And he had a really, really, really rough call. And I was like, I don't know what to do to help you combat this situation. So let's go to the movies. So, you know, and I guess my dad is so, so wonderful. And especially now that I'm an EMS, being able to kind of, oh my gosh, what I'm at a loss for words, but he's able to kind of separate himself now and really, like help work through feelings and be able to being able to talk about it openly, I think, definitely helped me realize that I could do it.
Was there? Yeah. Was there a certain shift that you saw him? Like, was there something that made him become that way? Um, I think
just, you know, years of being in the fire service, you know, you see a lot. And I think over those years, when you're, when you're first new into EMS, and I, I can't speak for everybody, but I can, obviously speak for myself. When you're new into EMS, you're like, oh, my gosh, like, this is why I like this. You know, car accident, like, I don't think I'll ever be able to, like handle this, I don't think I'll ever be able to do this. But over the years, you kind of figure out how you can cope with seeing these things and handling them in different ways. And I think just watching my dad grow in the fire service and being able to, like, take those situations and figure out how to adapt and you know, I don't know, I guess, just being able to watch him grow in his.
Yeah, feelings, I guess. Yeah, yeah. No, I think
that if that's the right word,
You're making sense to me, because I feel like I can relate to what you're saying. I think there's maybe a certain times in our career, and maybe it's just a maturity as we go throughout our careers that we learn to handles these types of events, and this, you know, the trauma that we see, and some of us don't ever find ourselves, you know, in that space where we can deal with the cause, you know, and I think it just, it can add up and build up and right and lead to lots of different things, you know, PTSD and a host of other mental health issues. Maybe that's something that watching him go through probably accelerated your growth in that area. Yeah, to be able to deal with that type of stuff.
Yes. Definitely. Oh, my gosh, they're deciding that they wanted to play right now. But yeah, I think, you know, he's definitely had his fair share of difficult calls. And, you know, he's actually going back to school to help with first responders and coping with like PTSD, and, you know, mental health. And I think that is so admirable, like, there definitely needs to be more of that industry. But, yeah, just being able to see him do it. I think like, unconsciously or subconsciously, or whatever kind of word you want to use for that helped me be able to cope a little bit more easily with my calls. And I think having that conversation and being able to have that open line of communications with someone to talk about it in debrief is also incredibly helpful. I don't know what time they want to play.
No, I think I think you're I think you're right, I think it's being able to share that, you know, with other first responders and having that support group. Do you have that type of support group at both your your other jobs that maybe I do talk to people?
Yeah, I do. One thing, you know, that I've noticed? Well, I guess I'm trying to think back, like if there's a specific kind of like situation, but you know, I think after difficult calls, especially with like, our med crew members on like, the flight side, and the medical side, they do a lot of like, talking about difficult calls, if they've, you know, come across it, and they'll like sometimes come into dispatch, and they'll talk to us about it, because, you know, we're the first line of communication between that requesting agency and getting an aircraft launched to help with these patients. And, you know, we've sat and, you know, had text conversations with a couple of my crew members. Same with the fire department, there's like, there's a small handful few of people that, you know, if we have a tough call, we can actually like, reach out to each other and be like, hey, like, I need to talk about this. But overall, I really go to my dad a lot for different calls, because I know that he'd seen the things and I know that like anything I say, like he can handle it. And he knows just what to say, to help me kind of come down from it.
Sounds like he's gonna do a really good job after he finishes up school, because he's already on the right path. He's, he's found somebody already to mentor you, and probably all of his other, you know, his.
He's, like, I know that a lot of his firefighters that he works with, in the past, and probably currently have gone to him and like reached out for him reached out to him when, you know, they've had difficult calls, even though they don't even work at the same department anymore. They still kind of reach out to him and be like, hey, like, I really need to talk. And he's always opened up his ears and listened and help them, you know, sort out their feelings.
Yeah, do you like do you think? Yeah, do you think having I, I feel like just in my career, it's been a long time in my career. And I think in the, in the beginning of my career, it's just like, you know, you didn't know what to be okay with and what not to be okay with, like, sure. I've just seen some terrible stuff. And they're like you Okay, and I'm like, Yeah, I guess all right. Um, like, I, I mean, what, I don't know what else to feel like? Do you ever find yourself like that? When you start, um,
I did act like I did. And, you know, one of the instances like I can think of right off the bat, whenever you said that is, you know, I also worked for a little bit as an ER tech. And so while it's not like completely, like first line, there, it's the first line in the hospital. So you still see that initial response to a car accident, a shooting. And, you know, it's weird because of how many like just random like gang related shootings or domestic violence shootings that come in, like, you're like, oh, you know, this is a horrible situation, but it's so much easier to deal with. And then back in May of 2018, is actually when the Santa Fe shooting happened right down the road from us. And so I was actually working in the ER that day, I just picked up a shift to work in the ER that day. And we got, I believe, seven of the 10 wounded students. And so it was interesting to see for myself, how differently I handled, like the school shooting mass shooting situations versus just like a not everyday, like run of the mill shooting? Uh, yeah, probably a bad way to put it. But you know, it's, it was definitely interesting to see, you know, oh, I'm okay with this random gang shooting, but like, then I turn around, and there's this mass school shooting, and I was not okay. Yeah, after that.
Yeah, different circumstances play, you know, different roles in our, in our feelings? For sure. Yeah. And I think being, you know, you've had multiple roles. So you've, you've actually have seen it all kind of, in some ways, right? Like, yeah, dispatch human, and er, like, you've been out on the front line, that yeah, all in itself is like, just all completely different worlds in different perspectives, but then when you I feel like for you and you, like I'm in the ER that the feelings are a little bit different than when you're on the front line, they're a little bit different than,
yeah, you get in the ER, you get in a little bit more of like a relationship with the patient. Not to say you don't get one in the field, but you know, your transport times only so long, right. So you can have a conversation with the patient, and you can get to know them, and, you know, make them feel comfortable. But then once they get to the ER, you kind of done their Oh my God. And so then when you get to, you know, when they get to the ER, you get a little bit more time with them, and you can actually sit and you can talk to them and help them through being in the ER, I mean, it's such a grand process sometimes, depending on what you're coming in for. So being able to like sit and talk to someone be like, Okay, well, you're having chest pain. So here's what we're going to do. And here's everything that we're going to do, it's going to be a lot, we're going to do it all at once. So we're not kind of dragging this all out. So it's definitely different dynamics, working. In dispatch, we're actually you don't have any patient contact to working on the truck where you get a little bit of patient contact, and then in the ER where you get like a lengthy patient contact and kind of relationships. So definitely all phases.

Yeah, yeah. Yeah. Cuz I mean, bringing them into the ER, you're like, Okay, I think I know what was going on with them. And then you just, you drop them off and then you go, you know, to your station or to the next call in here. It's gotten better the information relayed back from a hospital or you go back to that same hospital you're like, oh, that chest pain turned out to be this. It wasn't actually chest pain or something. something else or the chest pain, this person was having a massive heart attack, we took him to the cath lab and it's Yeah, I think there's a lot in EMS that's coming along that way. I think it makes you feel better as a as an EMT, or medic or whatever, like to know what the results of that patient care was. And when you're in the ER, you get this kind of see like, hey, the medics brought in this patient, they thought it was this Yeah, no, but hey, we actually determined was totally something different. Yeah.
Yeah, it's very cool to be on like both ends of it. Especially like, as a newer, like, advanced EMT, like my skill sets gotten a little bit bigger. So you know, confidence is still building with, you know, being in the back and doing all these advanced, more advanced skills, I should say. So being able to, like follow up with the ER, like, give him a phone call. Or if I bring in the patient and be like, Hey, how is this patient that I dropped off? And they're like, oh, yeah, like, this was going on? And you did everything you're supposed to.
Yeah, yeah, it does definitely help build up confidence. And it helps you treat the next patient, you know, a little bit different, maybe that has some similar symptoms. When you're in when you're in dispatch, do you kind of paint your own picture of like, I'm getting this phone call. And I'm kind of painting this own picture in my head of maybe what the scene looks like. And then when you maybe talk to the flight crew after like, they describe the scene as it do, you often find it different than what you meant to be.
A little bit. So we're lucky to where we can we actually have radios that we can. Sometimes depending on the frequency that they're on, we can listen to our pilots and our med crew talk to like the ground units to get like the Elzey briefing and the patient demographics and kind of what's going on with them. And honestly, my favorite thing to do is, so Memorial, Hermann has this great program where we do hello Paja or so for any, like penetrating trauma, like gunshot wound, if it's to the chest or to the abdomen in the patient meets criteria, to go directly to the O R, they'll bypass the ER and just go straight to the O R. And so it saves patients so much time and get to that critical care so much faster. And so one of my favorite things to do, which probably sounds a little weird is to listen to the ground contact give a little briefing to our crew. And if I like if I like clue in and like I listened to the vitals and I listened to where the shoot or like the gunshots are and I'm like, you know, I bet this is gonna go to the O R. So like automatically, like, pull out the O R book and like, get everything ready. And I've been right like nine times out of 10 that they're going to go to the O R. And so then whenever the med crew comes in, I'm like, Okay, so tell me about the scene, like Paint me a Picture because I totally call that they're going to go to the straight to the award. It's
Yeah, I feel like that's a really rare, maybe in some bigger cities. But like in where you have that opportunity to go from the helo pad to the or not doesn't happen everywhere in the country.
It really doesn't. And I can't off the top of my head, tell you whether we're one, we are definitely one of the only air medical service services in the country that is able to do that. And it's I know, it's like a policy protocol that they've spent so much time working on. And we're very, very proud of it.
Yeah. When you not all hospitals are equal. Exactly. They all have different levels of different things that they can they can take care of. And, you know, when you're in Houston and probably in the heart of Houston, you know, the the hospitals are probably more capable of doing a lot more things in our area that I work in, you know, you're driving 30 miles to a trauma center that can do kind of like what your hospital does. Yes, you probably find that your other job.
Yes. And we're very lucky to have the Texas Medical Center right here in Houston because it's one of the busiest if not the busiest medical center in the country. There are a lot of hospitals in this small little radius of Houston. If you look at it on Google, it looks like its own little city. And so there's actually two traumas, two adult trauma centers into pediatric trauma centers and what makes Memorial Hermann so great is that, you know, if mom and kid are in a car accident, our aircraft can double load. So they can take both patients to the same hospital and both mom and or mom or dad and kid can be treated under the same roof. And so they don't have to be separated going to like a pediatric hospital like Texas Children's or they can both come to the same hospital and be taken care of and especially with all the traffic here aeromedical it's so helpful, especially during like rush hour times to get them to that higher level of care quicker.
Right. And it's incredibly traumatizing to the patients when they have to be split and sent to different hospitals. And the families like how am I going to split up my, my family to go to like whichever hospital I need to go to to? Right. Oh, be there. So that is pretty awesome. Yeah, it's,
It's one of a well, there's probably about 100 different things that are great about more Herman lifelight. But I can't even lift off the top of my head. But yeah, I think being able to transport, you know, families together, they, at the same time, like having those double in situations, and being able to send multiple aircrafts, double loading multiple aircrafts, that there's like a crazy enough scene, which we've done several times, but it's cool, I can't get over my jobs.
Yeah. That's awesome. Do you have something that kind of helps with your, with your mental health with dealing with all these different types of situations? Do you have a routine or I can go into your dad, which is pretty awesome. Yeah,
A lot of the times just going to my dad helps. Because he just knows how to do it. Actually, anyone in my family, like EMS wise, I can go to them and just kind of debrief or reach out to friends. But I, I have no shame in telling people that I go to therapy, it's a recent thing that I've started. And that has honestly changed a lot. In myself, I'm very much more open about how I'm feeling about calls, and how they affect me versus like prior, like, after the Santa Fe shooting, I was pretty open about how I felt about it, and how it kind of traumatized me and how like shootings after that affected me. But now that I'm in therapy, and I'm like, developing these different coping mechanisms, and, you know, realizing that it's healthy to talk about how you feel, and it's, you know, encouraging to talk to other people who are going through similar situations, it's definitely opened me up to be okay, with what I see on a daily basis.
Yeah, I think that's important to, to go to therapy. I wish I'd say this all the time and wish in the first year of everybody's career in the every year after that, they go to kind of go to least one session of therapy, because I, you just don't really know what's bothering you until you go.
Exactly. And I think in this is my opinion, and from what I've seen, I feel like a lot of times, especially in like fire, EMS, and even police officers, and probably even I mean military as well, they're, they're such like this macho man, you know, complex, not complex, but like stereotype, yeah, to first responders, where they've got to be big, bad and tough and hide their emotions, and they can't talk about it. And then, you know, you turn around and you look at the suicide rates and first responders are skyrocketing, because I just feel that people aren't comfortable enough to talk about what's going on and how they're feeling. And I wish that there was more of that.
Is that because Is that because you think they're feel like they're getting judged?
I think sometimes, you know, people, especially guys, I mean, you know, sometimes guys are like, Oh, I don't like to talk about my feelings. Right? And that goes with like everyday life. You know, they're like, I don't feel comfortable talking about my feelings, and then they don't, and then they suppress them. And that, you know, there's these hidden demons almost that build up. And I don't think that they realize that they do until they do. And then you, like, hope that it's not too late. But sometimes it is. And, you know, it's it's heartbreaking to see that there's so many people that don't feel comfortable. Right, expressing, hey, this call was really hard for me. I need to talk about it. And then, you know, taking the proper steps to open up. And yeah.
And I think quite often we're like shocked at that person took their life like people didn't see that coming because they masked that so well. Or like you said maybe their demons just rise up so fast that that they have no way of dealing with them or don't know probably the way to deal with them.
Yeah. Get off my train of thought for a second but yeah, you know, you You said that perfectly like masking their feelings like, you know, you go, you see these people for 24 hours, 48 hours at a time. And so you only see what people want you to see. Right? So they could come to shift and be, you know, quiet, but is that their normal demeanor laid quiet because, you know, it's a 48 hour shift, and they don't really want to be there, you know, it's sunny, they're at work, you know? And then, you know, they get off these shifts, and they're struggling mentally, and there's no way of knowing that in the short block of time that you see these people. Yeah. Because they're different at home versus where they are at work. Sure. And I think a big thing that citizens probably forget is, we have personal lives. We're human too. Like, yeah, it's pretty much impossible to check your emotions at the door, about what else is going on in your life. And I'll hear like, you know, somebody got pulled over. And then they're like, Yeah, this officer pulled me over. And he was a jerk. And I'm like, I he might have been, he might have been injured. You don't know what call he had before that. Right? Or, or how you know, what's going on in his home life? And that's really right. I get that when I don't want to make excuses, but it's just like, we are humans too. Yeah. Yeah.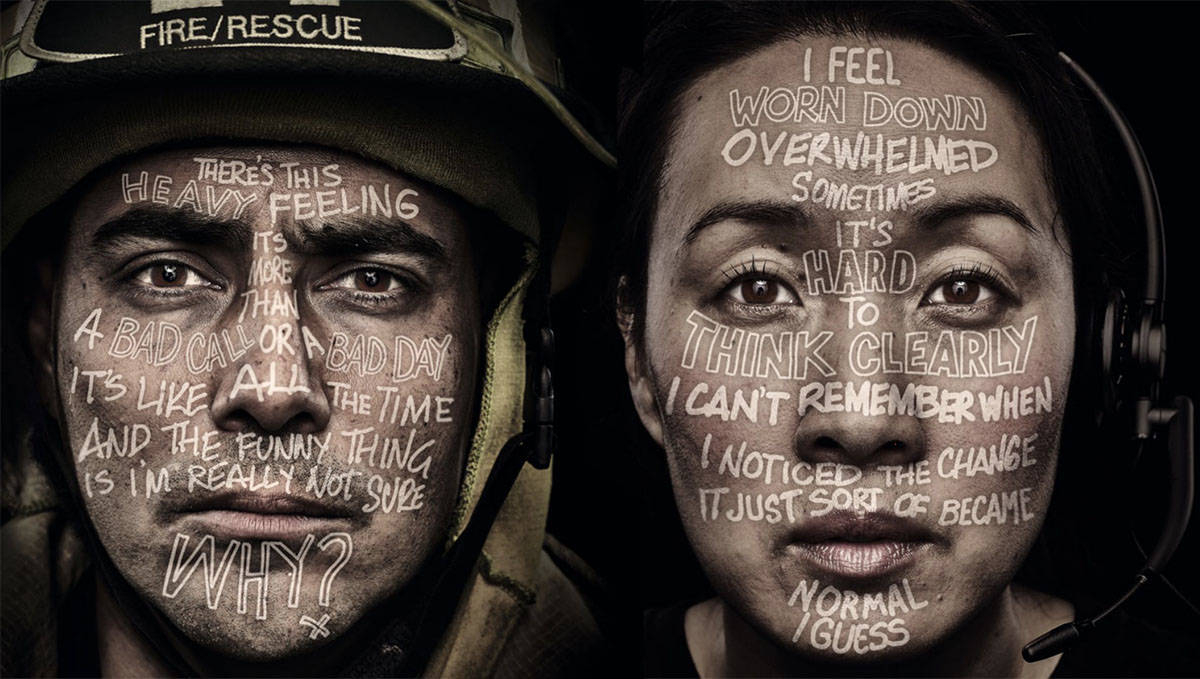
Yeah. And I think a lot of people are seeing that now with like, the pandemic, I think that really shined a light on, you know, EMS, fire, police, healthcare, like workers, like nurses, CNAs doctors, like, I mean, obviously, you know, people know what we do. But a lot of the times, it's like, you know, you're in the ER, and like, some person's complaining that they don't have a pillow. Meanwhile, you're doing an hour of CPR trying to bring someone back to life. And it's like, you don't realize that, like, we've got so much stuff going on, and that we can only do so much at a time, right. But yeah, I think people do really forget that we are humans, outside of like our job. And my favorite, not my favorite thing, but my least favorite thing I should say is when people were like, well, what's the what's the worst thing you've ever seen? Yeah. Like you want me to relive my worst trauma as an entertainment to you? Like, I don't? That doesn't make sense to me. So I always, I always, you know, politely declined to tell them. Because I don't think you actually want to know the worst thing I've seen. Yeah, and I definitely don't want to relive telling you.
Yeah, and I think I'm right, it brings up emotions from from call and it's hard to re-shift those emotions back down, after you know, told somebody like what your what your worst call was. I think that's something on I think people on listening that aren't first responders, sometimes to the podcast, they, they really want to know those things. And it just, it just brings up emotions that aren't needed to be to be brought up. And yeah, as you can imagine, we we've, if you've been in fire, EMS, law enforcement in the military, what you've seen on TV in the news, yeah, you've been right there for those things. And what you're seeing is probably, you know, a lot of times, like on the news is not accurate, either. But oh, yeah. It's just like, yeah, they're horrific details that, you know, nobody nobody wants to share.
Yeah. Anyway, not the easiest thing to do. I think very relive that.
Yeah, to relive that, yes. I think a good place for I think as first responders maybe to do that as right therapy is to, depending on type of therapy, you go to some therapies, not talk therapy, there's different types of therapy, where you don't really have to rehash those type of calls, which I'm a fan of, because I I'm not a huge advocate myself and just talk therapy, like the other day, where there's little bit of talk and little, you know, EMDR, or AR T or different types of stuff where I'm not just constantly pouring out my my guts and, you know, releasing all my emotions.
Yeah. Is there some good I'm totally the opposite. I love talk therapy. Yeah, because I in normal life cannot express my feelings very well. But then like, I go into, like this therapist, and I'm like, let me spill my guts to you. And I don't know why it's so easy to talk to you versus like people in my regular day. Because like, that's who I should feel comfortable with to to, like, express all these emotions, but I can't say I'm gonna go to therapy and just like, dump on you. And it's wonderful. For me, at least. Yeah, and
It's right. It's just therapy, whichever type therapy you find it has to be the right fit for you. So maybe if you don't like one type, just don't give up like five different therapy that works for you or a different therapist. We've had different therapists. Yeah, on the podcast, and they're just like, you are not going to like every therapist that you go to just like, like every dentist you go to, like you don't like every time you go do like, you have to sometimes bounce bounce around a little bit to find what really works for you.
Exactly. So that's my thing. Just don't give up. Yeah, find a therapist, if that's what you choose to do. I mean, it's not an easy task to find a therapist that you feel comfortable with, or that you feel is actually doing good for your mental health. So I don't want people to be like, deterred from therapy, because they went to one therapist, and, you know, they didn't like them. Like, you got to keep trying on different shoes until one fits.
Yeah, I think you might have more success in just in my feeling is just finding somebody that may have a little bit of an idea about what goes on in your job to kind of maybe a little bit relates and pull those questions out of you or understand the emotions that you're having.
That no,
I've heard of a couple of experiences of guys going to therapy and then spilling their guts, and then the therapist is crying with them. And I'm like, I don't know if I want that either. Yeah,
yeah. Yeah, it definitely takes a little bit to find one that like, completely understand what you do. And I wish that there was like, more access to those people. You know, that they were there more of them? I should say, yeah. Yeah. Because they're very few and far between that are actually like specialized in first responders and being able to help with the PTSD that comes with the different calls.
Sure. Sure. What, what advice do you have for someone getting into the EMS services?
So actually, I get this question a lot. Because a lot of people come to me, and they're like, Well, I don't know if you know, EMS is what I want to do. And I'm like, Well, I didn't know if EMS was what I wanted to do, either. But I signed up for the class and it was great. I would say definitely, if you're not sure about it, the first step would be to reach out to your local college, or wherever the program is held, and talk to the teachers or the directors and reach out to local departments or agencies that you want, you know, to talk to you and see like, hey, is this a good fit for me, because you know, talking to people who are actually in it is going to be your best bet to find out if you can do it. Yeah, as far as like starting out. My biggest thing is, don't be afraid to ask questions. Or admit when you don't know something. One of my biggest downfalls when I first started was I was very, very nervous and didn't want to admit when I didn't know how to do something. And so it would take a little bit for me to figure it out. And then I'd have to like, run back to my dad and be like, Dad, how do I do this? And then like, run back to work and be like, Okay, I can do this, instead of just like owning up to it and being like, you know, what, I don't know how to take a manual blood pressure properly. That was my biggest thing. I could not take manual blood pressure when I started to save my life, or somebody else's. But luckily, I had great instructor great field training officers that like sat me down and be like, here's how you do it in a easy way. And once I realized that I could actually like, sit down and be like, I don't know everything. And I'm, it's okay to not know everything when I first started, because none of you guys do. And I think a lot of the times, whenever you're new especially in first, like first responders in general, you know, you have this mentality that you've got to be big, bad and tough, and you've got to know everything, but it's completely okay to not know everything, because you're not exposed to those types of things when you're in school. And so it's gonna take like a long time for you to like, build up everything that comes in EMS and knowing how to treat and handle all the different components that comes with being a first responder. It's not like a nine to five job where you do the same thing every day. Don't call every time.
Right, right? Totally different than you could not one chest pain is the same as the last blast chest pain. Even, you know, patients are different family dynamics are different. There's just always so much different. Do you think we're gonna put you on the spot here a little bit and I told you I wouldn't.
We'll see how it goes.
Yeah, no. It's just Like, do you think there's just too? On both sides? I guess there's two sides of things. One, maybe we feel like as a first responder, we're supposed to be perfect. So we don't want to ask questions to somebody else. And maybe there's another part that we're afraid of being judged. If we do ask any questions. I'll personally, I been doing this for 32 plus years, I do not know everything. And I will continue re-learn through out, you know, until I retire, there's just no way to know everything, everything. I feel like sometimes they give us like a complex or like, I feel like I should know everything.
Oh, for sure. And I was totally like that, especially like, you know, when I started basic, and then when I got my advanced, I was like, Oh my gosh, like, I'm nervous to even like, say that, I don't know how to do it. But I have one really great friends at my 911. Department. He's a paramedic, and he's been a paramedic for years. And I actually opened up to him one day, and I was like, You know what, I'm afraid to work with a basic as the like, as the advanced or the higher patch on the truck, because like I have not been exposed to at all as an advanced and actually, just the other day, I had a situation where I walked in, and the patient was in cardiac arrest, or respiratory arrest. And I had to like initiate, you know, a whole code situation. And I was like, I don't know what to do. Yeah. I mean, like, I knew what to do. Yeah. And I'm like, yeah. I don't know what to do. Like, I need, like, I need a paramedic here. And so luckily, they cleared a call, and they were able to get to me within like minutes of it, of us even being on scene. And so I think in those moments, I've definitely opened up to the fact that I don't know everything, and then that, that's okay. Yeah. And so I go to, you know, this friend of mine all the time, and I'm like, Hey, I have a question. And he sits there, and he'll explain it to me, which I wish that there was a little bit more of because I have had people come to me, especially like on Instagram and been like, hey, like, I had this situation. And I don't feel comfortable asking, because I feel like I'm going to be judged for not knowing it. Sure. You know, our, like, our programs aren't that long. My basic program was five months long. My advanced one was six months long. You know, it's not a very long time to be in school. And you have to know how to treat just about everything. Yeah, yeah. And so it's gonna take years, like you said, you're still learning. Everybody's still learning. I think everybody will learn from the day they start to the day they end, like, there's never going to be a situation where you're like, you know what, I think I'm done learning. I think I know everything.
Yeah. Yeah, that's an ego comes in. I think when you do that,
Yeah, I think they're neat. I hope that one day, there's gonna be a lot less of people who are uncomfortable, and asking questions, because there's gonna be more comfort in the people above you, the people that have been there longer, you know, it's, it's got to be a family, we're all in this together, we're all going to see the same stuff. And the same calls. And we can't be against each other. Because this person's new and this person has been here for 20 years.
Right? I think the biggest issue that I see with that is we're supposed to mentor and coach these people that are below us, or less knowledgeable, or whatever the situation is, but not one textbook that I've seen as a paramedic, or EMT, or firefighter that really dives down into telling you how to be a paramedic mentor or a fire mentor, or there's nothing in there. And not just because you've like, done for a long time doesn't mean you're a great mentor, or a great person tell someone how to do things.
Yes. Not all teachers are great teachers like, and that's not nothing to, you know, teachers or anything. But in general, you know, I will admit that I don't like if you put me in a situation like you've been an EMS for six years, like you can go ahead and train this student, I'm going to be like, you don't want me training the student? Because I'm not going to be very good at it. Yeah. I mean, I can teach them some things. But I, you're asking the wrong person. And I think there's a lot of people that are trainers just because of the time that they've been in EMS, that probably shouldn't be because, yeah, you know, they've got this well, you should know everything complex to them. And it's kind of steering people away from wanting to do you know, fire EMS, pulleys. Well, I don't know. Yeah. Because like, you know, they don't really want to do it because they're like, Well, I'm supposed No everything and because I don't they're making me feel like I had a kill your confidence here. Yeah,
Yeah, yeah. And actually this if he, I don't know if we'll be able to this book right here written by two paramedics out of Colorado. And it's a great book. It's called life and death matters. And it's about professionalism and decision making for first responders. So it kind of teaches you how to be to make one make those great decisions and how to be a mentor to new medics or new people and stuff like that. I think more books like that out there, and more people reading them will definitely help the films that we're in to, to do that, and more support by the departments to be like, hey, yeah, we should send you to nuts that have nothing to do with being a fireman or paramedic writer, we're gonna send you to this class about how to be a coach, or how to be an actor or how, how to do these things, and not just expect you to know how to do these things? Well, when you haven't been trained.
Know that, that would definitely, I feel, help a lot of different departments and agencies to be better and have people stick around. I think that's why turnover rate too high. In especially EMS, like people don't want to work with people they don't feel comfortable with. And you can't really take care of patients if you don't feel comfortable with your partner. And if you have a mentor that's like tearing you down every step of the way. It's not easy.
No, because you never you don't ever have the confidence to make the right decisions, or you're always wondering if you made the right decisions. And when that's in the back of your head. I feel like it's really hard to make those perfect decisions. You know, it just not gonna happen.
It definitely is. And that's what you know, so great about, you know, oh, my friend Jeremiah, like, and with our call the other day, you know, he's such a great mentor that like I panicked. And he even told me, he's like, I saw this, like, sense of relief come over when you saw me on scene. And I was like, I can tell you that there is relief that came over me when I saw you because I knew, not only did I have the support I needed for this patient, but you also helped me through things. If I'm like, Hey, and you know, for instance, I had like an on that call, I have started one IO in my entire EMS career. And so this was going to be the second IO that I've ever done. So he actually, we had multiple hands going on this patient, but he actually like took a second and like confirmed my placement with starting this IO because I was like, I don't want to have to drill this guy again. So I was like, can you just take a second and confirm that I'm doing this right. And he did. And you know, it was very comforting to have that. Especially on a critical call, you know, because it only takes two seconds to do. Yeah, just be like, yep, you're right. Go ahead. Yeah.
Yeah, and that's good. But we need more of right. And you are going to remember that a lot easier than if the opposite of that happened, you know? So I think just taking those few seconds, it's not going to change the outcome of the patient's care by just saying, Yep, looks good. Way to go. Yeah. Aubrey, you've had a lot of great information. And I'm glad we could connect. And I know there's gonna be some people that are gonna want to reach out to you to maybe ask some questions in your spare time when we do when you're not sleeping, or studying or whatever. Where can people find you? Yeah.
Well, I'm mostly on Instagram. I just changed my handle back to messy buns in scrubs. So anybody can reach out to me through messages through comments. I'm always looking at that stuff. And I love when people reach out to me and ask me questions, because there are a lot of people that don't feel comfortable, go into their FTS or to their supervisors. And, you know, they feel comfort in talking to a stranger online as weird as that sounds. Because it's not someone who knows you in everyday life. So you can be like, Hey, you're probably not going to judge me on this. What about this question? And so I've had a lot of people come to me, like, brand new out of basic or, you know, looking to start, and they reached out and just ask questions, and I've sat there and like, talk them through, and then it's great to see like six months later, when they're like, I just finished my basic program and like, thank you so much for giving me the confidence to go and do it. And I'm like, that's amazing. I love when people do that. Yeah. And mental health. A lot of people reach out to me about mental health and ADHD. That's one thing I'm big about sharing too. Because there's a lot of different aspects to mental health too. So yeah, never hesitate to reach out to me. I love talking to people.
That's awesome. No, that's that's very much appreciated and very much needed. And I think that says a lot about who you are if people are willing to reach out to you like that. Yeah. Well, thank you so much for being on the podcast today.
Thank you so much for having me. I had a lot of fun. Yeah,
Me too. Me too. Thank you.
Thank you so much for listening. For those of you that didn't know I'm a mindset coach. And with all this going on in the world right now, I want to give back that's why I'm giving one free month of my coaching to one person. If you're interested in learning more, please go to the website and leave me a voice message or go on to @enduringthebadgepodcast on Instagram. Or you can also find me @firingandfuelcoaching on Instagram as well.
Outro
Don't forget to rate and review the show forever you access your podcasts. If you know someone that would be great on the show, please get a hold of our hosts Jerry Dean Lund through the Instagram handles at Jerry Fire and Fuel, or @enduringthebadgepodcast. Also by visiting the show's website, in during the badge podcast.com for additional methods of contact and up to date information regarding show. room remember the views and opinions expressed during the show. So we represent those of our hosts, and the current episodes guests.
Everyday Heroes Podcast Network
This podcast is part of the everyday heroes podcast network, the network for first responders and those who support them

Bree Johnson
I am a current AEMT who has been working in EMS and in the hospital setting for six years now. I am a third generation EMT, following in the footsteps of my grandpa, mom, dad and even uncle! I am currently in school for respiratory therapy but plan to continue my EMS career even after school.










